Spring has officially sprung so what better way to celebrate than by trying out some delicious and healthy recipes perfect for this season? Taken from the recently launched cookbook, ‘Eat Well to Age Well’ by Beverly Jarvis.
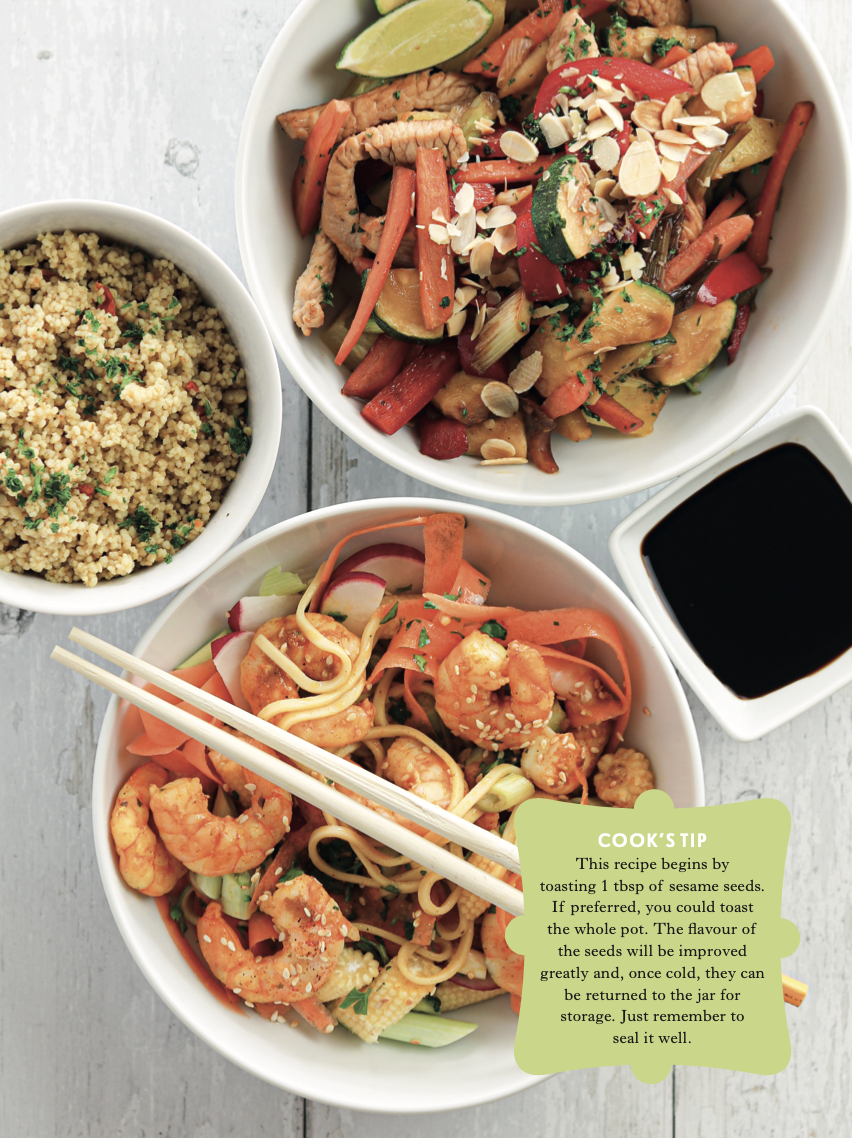
King Prawn Noodle Salad Bowl
Serves 2
This is a great fish dish with Oriental flavours. It is easy to prepare and speedy to cook – a tasty and nutritious meal, which looks pretty too.
INGREDIENTS:
1 tbsp sesame seeds
150 g wholegrain noodles
3 tbsp olive or rapeseed oil
250 g shelled raw king prawns
1 rounded tbsp red curry paste
2 tsp runny honey
2 tsp fish sauce (I like Blue Dragon)
1 tbsp light soy sauce
1⁄2 lime, juiced
1 tbsp freshly chopped coriander
1 carrot, shaved into ribbons
2 radishes, sliced
4 baby sweetcorn, sliced thickly
2 spring onions, chopped
EQUIPMENT:
You will need a chopping board and knife, a large saucepan with a lid, a large frying pan or wok, a dinner plate, vegetable peeler, citrus juicer, tablespoon, and teaspoon, a small bowl, a wooden spoon and 2 shallow serving bowls.
NUTRITIONAL NOTE:
The prawns make a valuable contribution towards your RDI for protein as well as providing vitamins A, B6 and B12 plus calcium and iodine. Prawns contain quite high levels of cholesterol but a 1996 study, compar- ing a low-cholesterol diet with one that included eating prawns every day, found that the prawn diet increased HDL (‘good choles- terol’) and significantly decreased triglycerides while only slightly increasing LDL (‘bad’ cholesterol). Prawns also have a good balance of essential fatty acids with almost three times more omega-3 fatty acid than omega-6 fatty acids (see page 17). The vegetables contribute fibre and antioxidants.
INTRUCTIONS:
- In a clean, hot frying pan, over a medium heat, toast the sesame seeds for about 1 minute, stirring frequently, until golden, then transfer to a plate and set aside.
- Cook the noodles according to the packet instructions, normally about 5 minutes. Drain.
- Meanwhile, heat 1 tbsp oil in a wok or large frying pan over a medium heat. Add the prawns and stir-fry for a minute or two until pink all over.
- Add the curry paste and stir-fry for a minute.
- Add the honey and fish sauce, with about 4 tbsp water, and stir and heat for 2 minutes.
- In a small bowl, make the dressing by combining the soy sauce, lime juice, remaining oil and coriander.
- Combine the drained noodles with the carrot, radishes, sweetcorn and spring onions.
- Pour the dressing over the noodle mix and toss everything together.
- Serve the noodles, divided between the two bowls, with the prawn curry poured over, and topped with the reserved toasted sesame seeds.
Vegetable Risotto With Roast Tomatoes
Serves 2 – 3
Risotto makes a filling and truly delicious main course, which is easy to cook if you use this largely baked-in-the-oven method. It is a great complete meal, with bags of flavour in both the risotto, which is cooked in vegetable stock and the tangy tomatoes. I usually prefer using brown rice for extra fibre and vitamins. However, there are times when a creamy, satisfying risotto just has to be made with arborio rice. You will find it in supermarkets, alongside long-grain rice, sometimes just labelled ‘risotto rice’. However, don’t stress if you can’t find arborio risotto rice; just use long-grain white rice instead. It won’t be exactly like an Italian risotto but it will still taste great, I promise!

INGREDIENTS:
1 tbsp rapeseed or olive oil 1 medium-size red onion finely chopped 1 stick celery, finely chopped
1 medium-size carrot
sliced 125 g sweet vine tomatoes, quartered, or halved if using cherry tomatoes
Salt and freshly ground black pepper 150 g arborio risotto rice, or long grain rice, rinsed and drained
1 tsp freshly grated root ginger
1 clove garlic, crushed
650 ml hot vegetable stock
3 tbsp white wine, or dry cider, optional, or use water
5 tbsp frozen peas
1 small red or yellow pepper, de-seeded and chopped
EQUIPMENT:
You will need a chopping board and knife and a large frying pan with lid which is both hob- and oven-friendly. (If you are worried about the handle, triple wrap it in tin foil, before transferring the pan to the oven.) Also a teaspoon, tablespoon, wooden spoon, roast- ing tray, measuring jug and cheese grater.
NUTRITIONAL NOTE:
The rice makes a valuable contribution towards your RDI for carbohydrate. The tomatoes and bell pepper add fibre, antioxidant polyphenols and vitamins A and C.
TO SERVE:
50 g vegetarian parmesan cheese, freshly grated. Handful basil leaves, chopped. The oven-roasted tomatoes.
INSTRUCTIONS:
- Pre-heat the oven to 210°/190°C fan/gas 6.
- In a large frying pan, heat 1⁄2 tbsp oil over a medium heat, until shimmering.
- Stirring frequently, over a medium heat, fry the onion, celery and carrot for 5-7 minutes, until softened.
- Meanwhile, put the tomatoes onto a roasting tray. Drizzle them with the remaining oil, season with salt and pepper, then roast for about 15 minutes.
- Stir the rice, ginger and garlic into the pan with the vegetables.
- Increase the heat and add 300 ml of the stock, with the wine or water. Stir well and bring to a rapid boil.
- Cover with a lid and transfer to the oven, above the tomatoes
- Bake for 15 minutes.
- Remove the risotto from the oven and transfer it back to the hob.
- Gently, stir in the peas and the red or yellow pepper, with the remaining stock.
- Cook uncovered, stirring, over a me- dium-high heat, for 5-7 minutes or so, until the rice is al dente and the peas and peppers are just cooked.
- Remove from the heat, adjust the sea- soning if necessary, then serve, sprinkled with the basil, and the parmesan cheese, accompanied by the roasted tomatoes.













 services.
services. Both countries are affected by humanitarian crisis and the health systems are very fragile and weak. Due to the high level of insecurity caused by non-state armed groups, transporting contraceptives, medicines, medical supplies and equipment to reach the last mile is a major challenge. The weak health systems were equally hit by the Covid-19 pandemic, epidemics (including Ebola in the DRC) and natural disasters (including the Nyiragongo volcanic eruption in the DRC).
Both countries are affected by humanitarian crisis and the health systems are very fragile and weak. Due to the high level of insecurity caused by non-state armed groups, transporting contraceptives, medicines, medical supplies and equipment to reach the last mile is a major challenge. The weak health systems were equally hit by the Covid-19 pandemic, epidemics (including Ebola in the DRC) and natural disasters (including the Nyiragongo volcanic eruption in the DRC). One of the things I do in terms of community and ‘giving back’ is the work I’ve been doing with my local hospice. I’ve volunteered with
One of the things I do in terms of community and ‘giving back’ is the work I’ve been doing with my local hospice. I’ve volunteered with  some 11 miles away. She was eventually trapped in a driveway. The police took her in, got details from her ID tag and contacted Love Underdogs and me.
some 11 miles away. She was eventually trapped in a driveway. The police took her in, got details from her ID tag and contacted Love Underdogs and me.
 I also talk about Nordic walking – using poles – which I boldly describe as ‘perfect exercise’. It is very clever – it elevates the heart rate, gives the lungs space to work, improves the posture, protects the joints, strengthens the bones, supports the balance (pain and numbness in your feet is a common side effect of chemo). It helps reduce the risk of, and manage, a condition called lymphoedema, helps rebuild upper body strength and uses 95% of your body’s muscles.
I also talk about Nordic walking – using poles – which I boldly describe as ‘perfect exercise’. It is very clever – it elevates the heart rate, gives the lungs space to work, improves the posture, protects the joints, strengthens the bones, supports the balance (pain and numbness in your feet is a common side effect of chemo). It helps reduce the risk of, and manage, a condition called lymphoedema, helps rebuild upper body strength and uses 95% of your body’s muscles.
 Parkrun
Parkrun