
Blog post written by Sarah Russell, author of The Bowel Cancer Recovery Toolkit.
Over a decade has passed since I had my own stoma surgery. And if someone had told me that 10 years later I would have a book translated into Chinese and I would be training ostomy nurses in China on Zoom, I would never have believed them.
Life really does take an incredible path sometimes. Here’s the timeline of how I went from ‘patient’ to ‘global expert’…
11 years ago
I went through abdominal surgery to remove my bowel and have a stoma formed, after suffering a life-threatening bowel perforation. I would need to use a colostomy bag fo
r the rest of my life. In most cases stoma surgery is life saving and life changing, and that was certainly true for me. I underwent 5 major operations over 18 months and it would be fair to say it was a difficult time. I had 2 young children and was a competitive athlete at the time. The surgeries floored me and I remember wondering if I would ever be able to go cycling or running ever again.
Lying frail in my hospital bed I asked about exercise, abdominal rehabilitation and whether I could run and do sports again now I had a stoma. My questions went unanswered. Nobody seemed to know what to do.

9 years ago
I managed to rehabilitate myself, get fit, retrain my abdominal muscles and return to running, cycling and the life I loved. To date I’ve completed 37 marathons and have just run a 50 mile ultra-marathon in the UK.
But in doing so realised there was a huge gap in patient support, nurse/surgeon education and knowledge about rehabilitation and exercise after stoma surgery. Despite my best efforts this hasn’t changed much, and we are still very much scratching the surface.
6 years ago
I started working with ConvaTec as their global exercise specialist and through our research in the UK, found that people who had their stoma due to cancer were reluctant to return to exercise and had very low levels of physical activity. I then trained in cancer rehabilitation to add to my MSc in sport/exercise science and 20 years of fitness rehabilitation qualifications.
4 years ago
I was working with a colorectal cancer patient (who was a keen runner and triathlete) and wanted to find an inspiring book for her to read about returning to exercise. I looked and couldn’t find one. So thought ‘Oh I’ll write a book then. That won’t be too hard’.
I contacted Hammersmith Health Books who took it on without a moments hesitation and then patiently waited whilst I wrote and re-wrote the book. It turned out writing a book is quite hard.
2 years ago (in 2019)
The Bowel Cancer Recovery Toolkit was finally published.
Let me tell you, if you’ve never published a book, it’s a terrifying process. Waiting for the first reviews on Amazon is utterly nerve wracking.
I hoped that people would find it comforting, useful and helpful. Which thankfully they have. Not only that but nurses and doctors have given it rave reviews and recommend it to their patients. That’s all I wanted and it makes me really happy to be able to help others. Read the reviews here.
During this time I continued to work with ConvaTec as a consultant and we developed an innovative nurse training course and the me+recovery training programme for patients.
For the first time patients could access professional advice on rehabilitation after stoma surgery and nurses could attend an RCN accredited (the only one of it’s kind in the world) course to teach them about abdominal exercises and safe activity for their patients. To date we’ve trained 350 UK nurses and many more around the world.
And so now today..
 My book has just been translated and published in Chinese (a first for Hammersmith Health Books). I honestly find this mind blowing, but probably unsurprising. As it’s clearly something that’s desperately needed.
My book has just been translated and published in Chinese (a first for Hammersmith Health Books). I honestly find this mind blowing, but probably unsurprising. As it’s clearly something that’s desperately needed.
Each year there are around 380,000 people diagnosed with colorectal cancer in China (with a population of 1.3 billion) and cases are rising quickly in people under the age of 30. It’s not a dissimilar picture in the UK, with around 45,000 cases each year and a sharp increase in younger people being diagnosed.
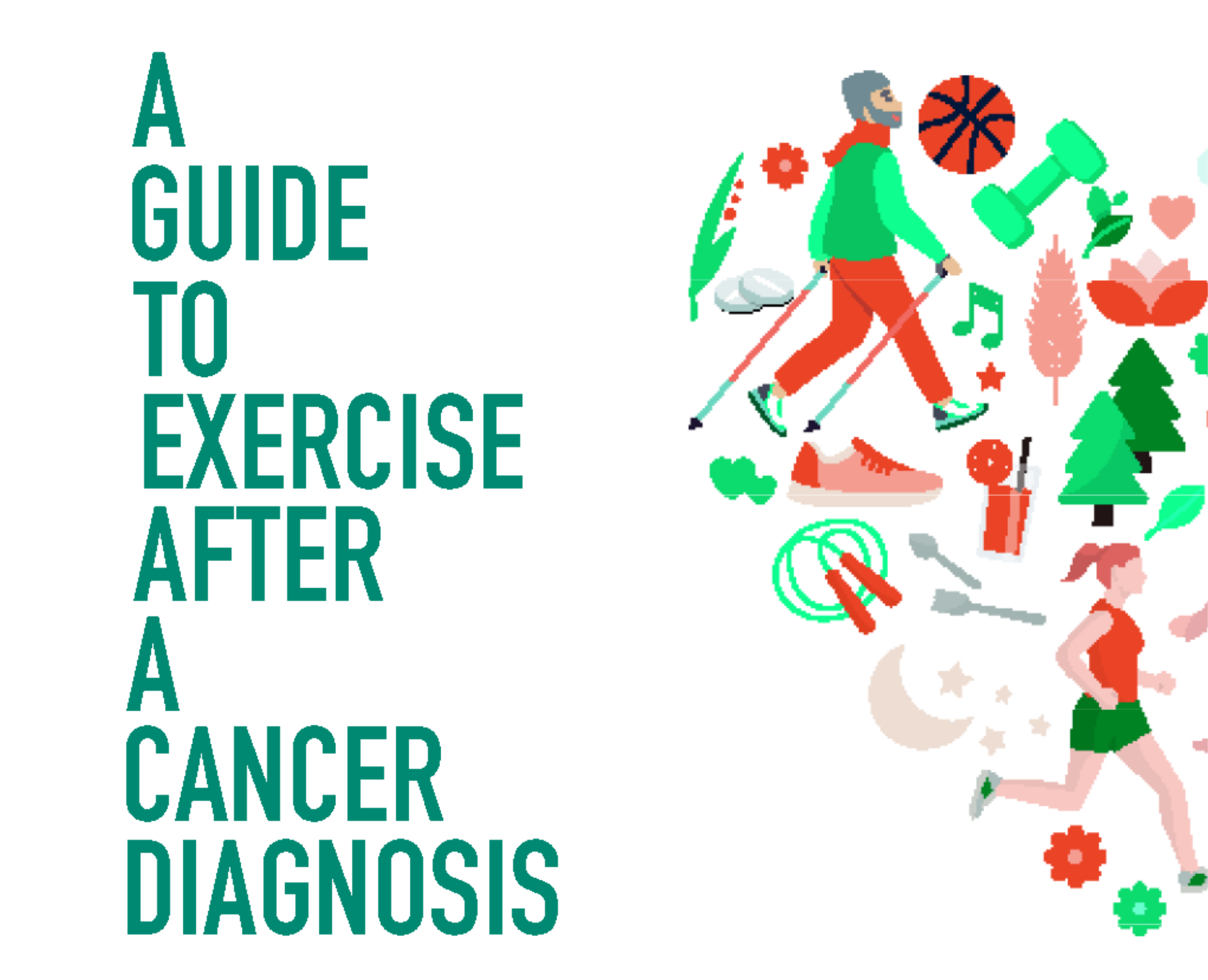
Even since publication of my book, the role of exercise in bowel cancer is becoming more and more important. Evidence is building to show that physical activity has a huge part to play in both prevention of cancer in the first place, but also in the role of recurrence. We now know that being physically active could reduce the risk of developing cancer (and it recurring) by around 30%.
If there was a pill that could offer the same thing, everyone would have it prescribed as a miracle treatment.
The exact mechanism as to why exercise is so effective isn’t yet fully understood, but it’s thought the anti-inflammatory effects of exercise combined with faster transit time through the bowel are the key physiological factors.
Having worked with thousands of patients, healthcare professionals and nurses over the last 6-8 years, I’m now hugely passionate about exercise and movement at all stages of bowel cancer prevention and diagnosis:
- As part of a healthy lifestyle to reduce the risk of developing bowel cancer
- As ‘pre-hab’ – getting fit for surgery
- As rehab – after surgery – aiding recovery and reducing risk of parastomal/incisional hernia
- As part of a healthy lifestyle AFTER a diagnosis of bowel cancer – improving mental wellbeing, confidence, physical strength and lowering risk of recurrence
- For people with terminal bowel cancer, potentially prolonging life and helping with symptom control
All of this is covered in the book, along with advice on diet after surgery and specific abdominal exercises after stoma surgery.
Of course each person will interpret the advice and information differently, exactly as they should. But the ethos of the book is for each individual to focus on their own recovery and develop the confidence to exercise safely in their ‘post cancer body’ regardless of wherever they live in the world and wherever they are on their cancer recovery journey.
And finally…
The most recent part of this story (and it’s certainly not over yet) is the most incredible and ambitious project put together by ConvaTec to deliver the me+recovery training programme to a global audience.
In August 2021, we delivered online training (via Zoom) for stoma nurses in China, Japan, New Zealand, Australia, Singapore, Malaysia and South Africa – all at the same time.
It comprised 4 x 3 hour sessions to a group of 60 nurses with simultaneous translation into Chinese and Japanese. With me sat at home in my little studio in East Sussex. And due to the time differences, some of the nurses were up in the middle of the night. That’s commitment.
It was incredible. The cultural differences and the clinical approaches were fascinating and so very different. But the outcome was that every single nurse involved wanted to do better for their patients. They wanted to learn how to help them rebuild their confidence, return to exercise and know how to do safe abdominal exercises after their surgery.
I didn’t think it could work. But it did. I’ve never experienced anything like it and it was an honour to be part of it.
In the book I write ‘My goal in writing this book is to try and help people, and to support, educate and encourage, and to start to change understanding and practice’.
And thanks to both ConvaTec and Hammersmith Health Books, that’s starting to become a reality.
Little by little we can start to change clinical practice around the world, give people better advice and enable people who receive a bowel cancer diagnosis to recover with confidence and live their best life.
For more information about me+recovery from ConvaTec Your home of stoma care advice, support and lifestyle tips. (convatec.co.uk)
For more information about my private practice www.sarah-russell.co.uk and my clinical Pilates www.theostomystudio.co.uk




 My book has just been translated and published in Chinese (a first for Hammersmith Health Books). I honestly find this mind blowing, but probably unsurprising. As it’s clearly something that’s desperately needed.
My book has just been translated and published in Chinese (a first for Hammersmith Health Books). I honestly find this mind blowing, but probably unsurprising. As it’s clearly something that’s desperately needed.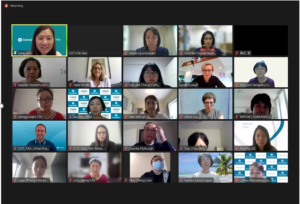










 Nori rolls (GF) (4 servings)
Nori rolls (GF) (4 servings) 
