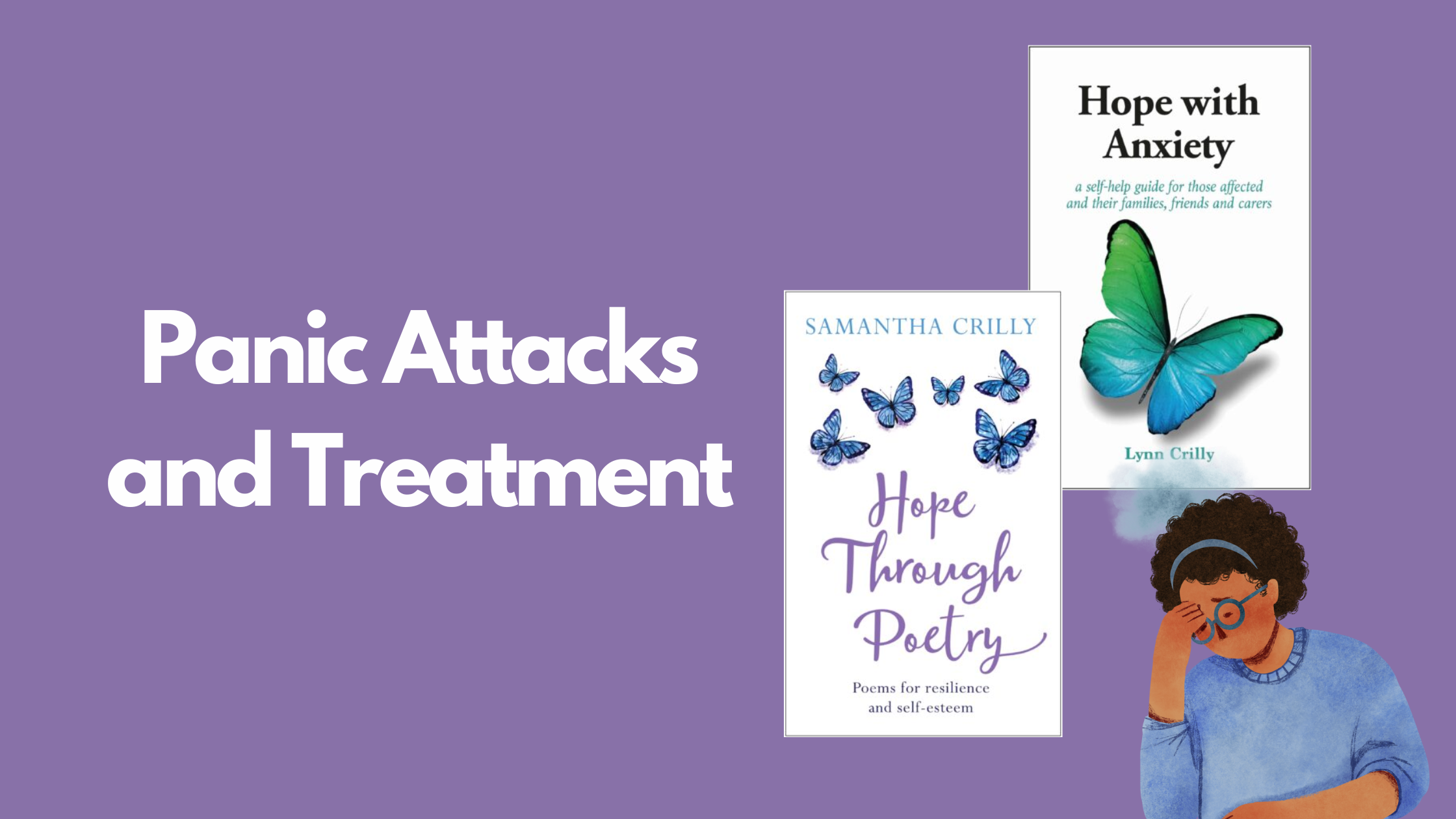
The following extracts are from author Lynn Crilly and poet Samantha Crilly from their respective books ‘Hope with Anxiety’ and ‘Hope Through Poetry’. The two pieces each give a personal perspective on the experience of panic attacks and look at some of the core causes of the condition.
Panic attacks and panic disorder
Anyone who has experienced just one panic attack will know just how frightening and debilitating they can be, sometimes seemingly coming out of the blue, without an obvious trigger. For someone with panic disorder, where these attacks occur with some frequency, the ripple effects on the way they live their life can be considerable.
Garry shares how he feels during a panic attack:
During a panic attack I would shake so much I could barely stand up. I had to sit down or lean against a wall to steady myself. Even though I knew it would pass, it was always very frightening.
Most panic attacks last between 5 and 20 minutes, but they can go on for up to an hour. Some people experience them once or twice a month, while others can be put through their effects a few times a week.[1]
A panic attack is terrifying and those who experience one can have an impending fear of death. It can typically cause a thumping, racing heartbeat, sweating, muscle weakness and a churning stomach. Some or all of these symptoms may be experienced, although the effects vary depending on the individual. Here is a list of some of the other physical symptoms that might be experienced during a panic attack:
- Faintness/light-headedness
- Nausea
- Chest pain
- Shortness of breath
- Trembling
- Hot flushes or chills
- Shaky limbs
- A choking feeling
- Ringing in the ears
- Numbness or tingling
- Feeling disconnected from one’s body.
Amy, who went through a period of regular panic attacks and severe anxiety, shares her experience:
I remember when I was 21, not long after my now husband’s father passed away and I went to Australia for a holiday on my own (I got really bad home-sickness, and ended up coming home from Australia after six days), I now realise that I was having symptoms of panic attacks and anxiety. At the time I had no idea, and the doctor thought I had an inner ear infection. I was off work for six weeks and I remember I couldn’t leave the house due to severe anxiety.
The psychological impact can be even harder to bear, with sufferers worrying they are dangerously ill, that they might die, that they might cause an accident and harm others, or might pass out and cause embarrassment or harm to themselves. These understandable terrors can have an impact on the way they live their day-to-day life, as people with panic disorder can start to dread or pre-empt their next attack, leading them to live in a constant state of understandable fear, which can cause more attacks to occur, leaving them locked in a seemingly unbreakable cycle.
Important note: At the same time, it’s worth noting that the symptoms of a panic attack may be caused by another underlying medical condition, such as hypoglycaemia due to insulin resistance, so it is always wise to consult a doctor, both to rule out any other cause and to get support in seeking help if it is a mental health issue.
According to the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders), in order to be diagnosed with panic disorder, the sufferer must have experienced more than one unexpected episode on a regular basis.[2] Mainstream treatment for panic disorder aims to ease the symptoms and lessen the number of panic attacks experienced. Talking therapies and medication are the main treatments for panic disorder offered by the NHS; depending on the severity of the symptoms, one or a combination of both of these treatments will be recommended by your doctor.[1]
- NHS Panic Disorder. www.nhs.uk/conditions/panic-disorder/
- Ankrom S. DSM-5 Criteria for Diagnosing Panic Disorder. VeryWellMind. www.verywellmind.com/diagnosing-panicdisorder-2583930
Glad you came
A poem about anxiety – by Samantha Crilly
It doesn’t add up like it did with high-school mathematics
Or have a narrative to follow in morning amateur dramatics.
You can’t find the square root of the problem, when the problem doesn’t exist
Or find reasoning for something when nothing was missed.
Anxiety manifests itself in so many different ways,
Often building and building over several days,
Detecting faults in situations that may never occur,
Preconditioning an event into one big blur,
Embarrassing yourself no matter what you do
On the main stage right in front of me and you,
Rubbing your knuckles, grinding your teeth,
Looking fine on the outside yet on fire beneath.
Heart pumping fast, echoing beats…
Dripping with sweat, hair slathered in grease,
Lungs tensed and twisted, unable to breathe –
If only you knew when you could leave.
But it’s okay I whispered – leave as soon as you need;
I’m so proud of you for just coming along.
To have stayed even for a little while makes you so strong.