The following is an extract from ‘The Fatigue Book’ by Lydia Rolley and looks at the importance of sleeping well in managing the effects of Chronic Fatigue Syndrome.
It would seem to make logical sense that, if you suffer from fatigue, at least you would beable to have a good night’s sleep, right? Well, as you have no doubt discovered by now, the fatigue does not play by the normal rules of life, and what your body is craving from a good night’s sleep is sadly often denied.
As humans, we spend approximately a third of our lives sleeping. That is quite a lot of time. Sleep is essential for our mental and physical wellbeing. Sleep contributes to the proper functioning of our body’s systems. Lack of sleep, therefore, has negative health consequences.
I have worked with many chronic fatigue sufferers who, although they sleep a lot, struggle to sleep well. From my experience, people either tend to over-think sleep issues, which can lead to increased anxiety about getting to sleep, or not to think enough about these issues,
which can lead to disordered sleep habits. Chronic fatigue sufferers who have sleep difficulties usually wake feeling unrefreshed. Some may not be waking until late morning or even into the afternoon. Often it is hard to get out of bed, as the body feels weighed down and heavy. The heavy feeling and sleepiness can continue throughout the day. Some people report feeling more alert for a few hours later on, often in the early evening. Almost a small window of hope, but this can be followed by difficulty switching off at night and not being able to get to sleep.
Changing your sleep pattern does not happen by chance. It does take a lot of patience, being intentional and very consistent. Concentrating on your sleep and developing healthy sleep hygiene habits together make the biggest difference to your overall health and ability to function and cope well. I have seen countless people transform their sleep habits and have witnessed the benefits. The change started when they chose to try something different.
Sleep difficulties can be complex and multi-faceted, but most can be solved. Ignoring sleep issues, and hoping they will go away, does not work. Trying to sleep for a few extra hours to fill the gap only tends to prolong the problems rather than solve them. When sleep is disordered, our bodies need to be retrained to know when it is time to sleep and when it is time to wake up.
What I have learnt over the years is that, even though some of these tips seem obvious, they almost need to be exaggerated, repeated and magnified in order to have an effect. Please keep that in mind as you start to put into practice the following tips, which will give you some useful starting points.
I have full confidence that you will benefit from healthier sleep habits.
Tip 21: Separate Day and Night Clearly
This is probably not your present reality and that is okay for now, but please keep this fact clearly in your mind as a goal for your future sleep pattern. The boundaries between day and night can get very blurred with disordered sleep. The more disordered your sleep becomes, the more unrefreshing will be your experience. Reintroducing clear boundaries will prevent further deconditioning.
This is the direction we are heading towards to regain a healthier sleep routine. For now, just be aware of your current day and night sleep routine by drawing a line on the chart below where you think your sleep pattern currently is.
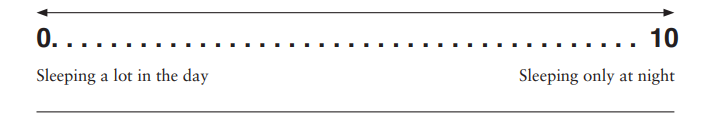
In the weeks and months ahead, be aware of how your current line gradually changes position and consider what has contributed to that shift. If you are sleeping excessively in the daytime and want to start changing that habit, see Tip 23.
Keep a Reflective Sleep Diary
The reason for keeping a sleep diary is to understand your current sleep situation and give greater clarity to what may need to change. This sleep diary is more of a reflective diary rather than a scientific measurement of your sleep cycles (such as on a sleep app). A reflective diary can be more useful in empowering you to make some changes.
In your reflective sleep diary (see Appendix 2, page 276) consider the following questions:
- What was I doing an hour before bedtime?
- How was I feeling in the evening?
- What time did I get into bed?
- How long did it take me to fall asleep? Why? Any reasons?
- Did I wake in the night? How often? Why? Any reasons?
- What time did I wake up?
- What time did I get up?
- How did I feel?
- How would I rate my night’s sleep out of 10? (10 being excellent.)
I would recommend only doing this for a week or two, no more than that. That is enough time to recognise any patterns of sleep and highlight any particular areas that need concentrating on.
Every few days, respond to the following statement:
Tip 23: Set an Alarm
This tip is not always popular but it is of the utmost importance. When you are exhausted and perhaps have no particular reason to get up, it may seem sensible to rest for longer, but this is counterproductive. Staying longer in bed does not help poor quality sleep. Sufferers frequently report feeling worse for going back to sleep. Seeking balance and retraining your body to learn a sleep-wake cycle goes hand-in-hand with managing your activities, pacing and rest.

I recommend that you try the following method to create an ordered sleep-wake cycle:
- Decide what time you would like to wake and get up, for example 8.00 am.
- Use a simple alarm clock with a silent tick.
- Place the clock somewhere that requires you to move to switch it off.
- Check your reflective sleep diary and set the alarm for the average weekly time you currently wake and get up – for example, it maybe 11.30am.
- Set your alarm at this time for a week, so that you get used to waking up with the alarm.
- Avoid going back to sleep – open the curtains, turn the light on, sit on the edge of the bed, put your pillows on the floor, etc.
- The following week, set your alarm for 30 minutes earlier.
- The following week, set your alarm for another 30 minutes earlier.
- Do this consistently for a few weeks, until you are waking and getting up at your preferred time.
If the 30-minute chunks are not successful, try 15-minute chunks of time.