Tackling depression naturally for World Health Day
Nutrition-related health issues seem to take an age to become part of accepted medical practice. The medical establishment requires comprehensive scientific evaluation, randomised trials and peer review before a new drug can be licensed, for instance. The pharmaceutical company has to weigh up the costs of research and development versus the potential profit to be made from launching a successful product that can earn a good return on their investment. (When you add in the factor that 80 per cent of their budget goes on marketing, it is clear the stakes are high indeed.) As real food is simply real food and can’t be licensed, branded or patented, there is little impetus for the medical community to fund costly research.
Medical research over the last couple of decades has, nevertheless, highlighted how an unhealthy gut can contribute to many physical diseases and these findings are becoming more accepted in mainstream medicine. Clinicians increasingly agree that the gut-brain axis also plays a crucial part in emotional wellbeing, including the development of conditions as diverse as chronic fatigue syndrome, depression and autism.
The Gut-Brain Axis
The gut-brain axis is a way of describing the interrelationship between gut health and brain health. The various aspects of digestion are controlled via the vagus nerves by a complex set of neurons embedded in the oesophagus, stomach, intestines, colon and rectum. The brain sends messages to all the nerves in your body, including the neurons that control digestion. All work efficiently enough until a person is anxious or stressed on an ongoing basis. You perhaps know for yourself that if you are feeling nervous your stomach can feel upset and queasy. The reason for this is that strong negative emotions, stress and anxiety increase cortisol and adrenaline, which then stimulate the sympathetic nervous system and shut down the parasympathetic system, which includes control of the gut. This causes a physical chain reaction:
* Reduction in pancreatic enzyme production
* Reduction in gall bladder function
* Reduction in the production of stomach acid
* Slowing down of peristalsis – the involuntary muscle movements essential for moving food efficiently through intestines for the absorption of nutrients
* Reduction in blood flow to the intestines
* Suppression of the intestinal immune system
In the short term, this allows the body to focus its resources on ‘fight or flight’ – a good survival mechanism. However, with ongoing stress and anxiety, this cumulative slowing down and suppression of the digestive process can, over a prolonged period, lead to a condition called ‘small intestinal bacterial overgrowth’ (SIBO). As the digestive process is compromised by stress and anxiety, the lack of stomach acid allows the stomach and small intestine – which should both be pretty much microbe free – to be colonised by unhealthy bacteria, and yeasts, causing foods to be fermented rather than digested. In addition to gas and bloating, compromised digestion leads to declining absorption of nutrients, which contributes to the loss of the co-factors needed for good digestion, and consequently further gut problems.
Now consider this situation lasting for extended periods of time. The integrity of the gut lining may be compromised, contributing to gut permeability (‘leaky gut’) that may be sufficient to produce chronic low-grade inflammation.
Chronic Inflammation
The inflammatory process includes the production of cytokines, chemical signals of inflammation that are carried by the blood to the brain. The cytokines can activate cells – so that the inflammation originating in the gut thereby causes widespread inflammation in the rest of the body, including the brain.
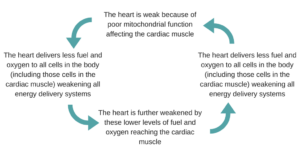
The impact of brain inflammation is that the brain has reduced nerve conductance which – guess what – shows up as depression, anxiety and stress.
This vicious circle can self-perpetuate and requires long-term changes to heal the gut, which in turn will help to heal the brain. This is done through changes in behaviour and improving levels of nutrition through changes to food choices. To improve your natural resilience to stress it is important to increase the amount of healthy polyunsaturated omega-3 oils in your diet, so look for oily fish, grass-fed meats and butter made from the milk of grass-fed dairy herds. Good plant sources include hemp seeds, linseeds, chia and some nuts and nut oils (macadamia, almond).
If you consider yourself to be depressed it will be helpful for your recovery to manage your stress levels, improve your sleep patterns and add nutritious and gut-healing foods into your regular eating plan.
Do bear in mind, however, that you may also need professional help if you have been suffering from this debilitating psychological disorder for some time. Please make sure you are accessing all the medical and psychological support you need. Try hard not to add isolation to an already challenging situation.
This blog has been taken from How to Feel Differently About Food by Sally Baker & Liz Hogon.